One morning about 10 years ago, JoAnn, then 52, was taking a shower when she felt something drop between her legs. Reaching down, she felt a slippery bulge. “It felt awful, like something was working its way out of my body,” she says. “I didn’t know what it was. I was scared.”
Later, JoAnn’s doctor diagnosed her with pelvic organ prolapse, a shockingly common condition that affects half of all women in their lifetimes.
“I think it’s probably the greatest hidden epidemic,” says Catherine A. Matthews, M.D., professor of female pelvic medicine and reconstructive pelvic surgery in the Department of Urology at Wake Forest Baptist Health. “Women will talk openly about stress incontinence, joking that they can’t jump on a trampoline anymore. But prolapse is this hidden mystery, and women get panicked. They wonder, ‘Do I have cancer? What is going on?’ ”
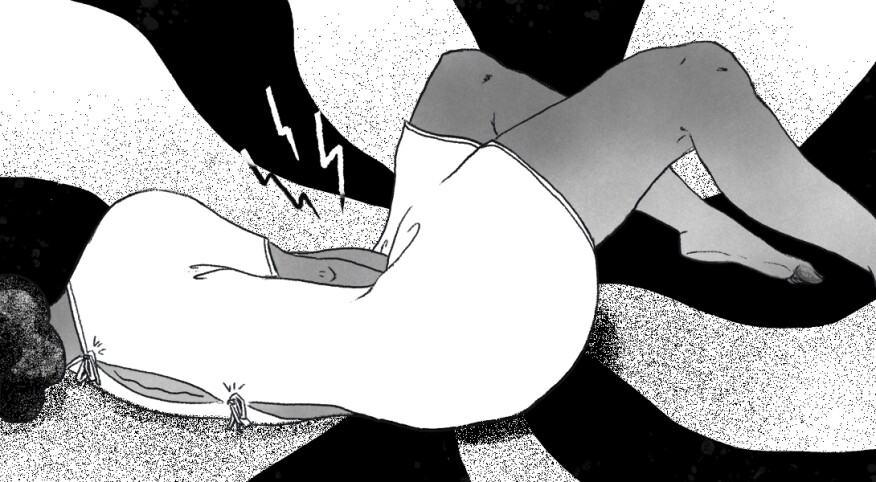
Prolapse happens when the pelvic floor muscles — which support and hold up your bladder, uterus, vagina and rectum — become weak and wobbly. When this happens, those organs can move lower inside the pelvis, sometimes protruding out through the vagina. You might also feel downward pressure or general discomfort, like you have a tampon in the wrong place, says Matthews.
Some women find it hard to go to the bathroom or have sex.
As a mother of two who had experienced long, intense labors, JoAnn was at a higher-than-average risk of developing prolapse. The most significant risk factor is delivering a baby vaginally — especially more than one baby. Other contributing factors include obesity, chronic heavy strain or lifting, smoking, and undergoing a hysterectomy. Still, a majority of women don’t notice symptoms of prolapse until menopause, when tissues shrink and thin.
“Women typically don’t become symptomatic until they have a bulge to or beyond the vaginal opening,” says Matthews. “If you had some relaxation of the pelvic floor, your gynecologist might mention it during an exam. But the first question would be, are you having symptoms?”
The good news is that only 20 percent of women will have progressive prolapse, meaning the organs continue to drop. If you aren’t having trouble with urination or bowel movements, aren’t persistently uncomfortable, and are able to have sex, then most doctors will recommend a “watch and wait” type approach.
“I think people are sometimes surprised to learn that they can live with it,” says Matthews. “It’s initially horrifying, but it’s like having a hernia. You’re not going to hurt or break something. It’s not your actual bladder that’s hanging down, it’s the vaginal wall.”
For those who do need treatment, physical therapy for your pelvic floor muscles is often a first step. “It’s not likely to resolve the prolapse, but intense pelvic floor exercises can prevent it from getting worse,” says Matthews. “There’s pretty good data that the weaker those muscles, the more likely someone is to progress from being asymptomatic to symptomatic.”
Your doctor may also prescribe a pessary, a rubber device that’s inserted into the vagina to provide extra support. Meanwhile, avoiding heavy lifting and losing extra weight can help reduce pressure on the pelvic floor.
“Intravaginal estrogen can also do a lot to mitigate the symptoms,” says Matthews. “The stretching of dry skin can sometimes be the most bothersome thing, and estrogen can help tremendously.”
About one in eight women will end up having surgery, which is often performed transvaginally, to return the organs to their original positions.
Matthews says the most important thing she tells her patients is to talk honestly about their bodies, especially as they age. “If men were experiencing this, it would not be such a secret,” she says. “It’s amazing how much women learn to cope with their bodies. But you don’t have to just accept something like this without figuring out what’s going on.”
LA Johnson









